Meet the ’24 Hour in A&E’ team
424 Hours in A&E at St George’s Hospital
After six series and seventy episodes at King’s College Hospital in south London, Channel 4’s award-winning series, 24 hours in A&E found a new home at St George’s Hospital in south west London.
Our A&E department is one of the most advanced and busiest in the world seeing on average 350 new patients every day.
The first of eight episodes filmed at St George’s aired on 30th October and the last just before Christmas 2014.
And ’24 Hours in A&E’ returned for a new series in the New Year!
Every Wednesday at 9pm on Channel 4.
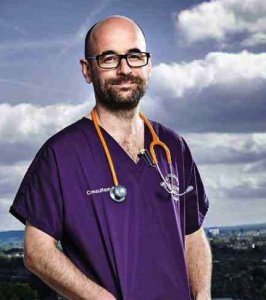
Getting to know Rhys…
 Consultant Rhys features alongside his St George’s colleagues in a couple of episodes in series 7 of ’24 Hours in A&E’ but it is episode 1 of series 8 (aired Wednesday 7th January 2015 on Channel 4 at 9pm) we get to meet him properly as he cares for a young boy suffering from a sports injury.
Consultant Rhys features alongside his St George’s colleagues in a couple of episodes in series 7 of ’24 Hours in A&E’ but it is episode 1 of series 8 (aired Wednesday 7th January 2015 on Channel 4 at 9pm) we get to meet him properly as he cares for a young boy suffering from a sports injury.
What is your role within A&E?
I’m one of the Emergency Department (ED) consultants. I have a special interest in children’s emergency medicine, so spend most of my time working in the Children’s ED.
How long have you worked at St George’s? Why did you want to join the team?
I’ll have been a consultant at St George’s for three years in February. St George’s offered a young, enthusiastic and vibrant team that I wanted to be a part of.
How many patients do you treat in an average day? What conditions / illnesses do they have?
We see between 350-450 patients in a 24 hour period. One of the things that I like best about working as a consultant in an Emergency Department is that I can be treating a new born baby one minute and then a 100 year old patient the next.
What did you think when they announced ’24hrs in A&E’ was going to be filmed at St George’s?
I was excited to hear that 24 Hours in A&E would be coming to film at St Georges. Kings hospital did such a great job, and the staff and department were depicted so well. I was pleased to think that the St Georges would have its own moment to shine.
Did you find it had any impact on your day?
I was surprised how little impact the filming had on my day. I got so used to turning up to work and putting on a microphone, and checking in with the “shop floor” producers. The TV company did a great job at making it really easy for me. My priority was always looking after the patients- that never changed.
What have you enjoyed the most from your experience of ’24hrs in A&E’?
It’s been great watching the departments reaction to the program. It’s definitely boosted team moral!
What has been your highlight moment of St George’s episodes so far?
It has to be the gentleman who had ketamine for his dislocated shoulder (series 7) and said ‘Everything’s gone wobbley bobbley’
What was the biggest challenge you experienced during the filming?
As consultants we were involved with consenting patients to be filmed. Sometimes this was difficult, but the production team were always there to help and support us.
What is the benefit of St George’s participating in a show like ’24hrs in A&E’?
It has been really important to show what a great service the NHS provides.
Is there anything that was or wasn’t caught on camera which you wish wasn’t or was?
There isn’t anything that I wish that had been caught, but I’ll tell you after the episode if there is anything that I wish that hadn’t been caught!
’24 Hours in A&E’ is back at St George’s for another series!
The RTS award-winning documentary series returns for a second series from its new home, St George’s in south west London, which has one of Britain’s most advanced and busiest A&E departments.
In this week’s episode (showing on Wednesday 7th January at 9pm on Channel 4) staff and patients discuss how A&E is a place where support really matters, but these days that support doesn’t always come in the form of a traditional family, but in all kinds of variations.
“I don’t expect to see a mother and a father or a husband and a wife,” says consultant Rhys. It’s more than being someone who just dishes out prescriptions and treatment. I’ve got all these people from all walks of life and I can learn something from all these people.”
13-year-old Will arrives by helicopter after colliding with someone during a game of baseball. He lost consciousness at the scene and medics are concerned that he may have sustained serious internal head injuries.
As doctors give Will a CT scan to find out how badly he is hurt, his mum Vicki describes what happened. “Will’s school had been trying to get hold of us to tell us to get to the school quickly,” she says. “They put him into the helicopter, he was tied down to the stretcher. You feel that it must be a lot more serious than a normal sporting injury.”
While they await the scan results, the medical team are concerned that Will hasn’t spoken since the incident and try to get him to talk.
Later, 20-year-old pizza delivery rider Chris is brought in to Resus after being knocked off his motorbike. He has sustained a very bad break to his right leg and doctors have to stabilize him before scanning the injury. While the medical team prepare Chris for surgery, he reflects on the accident and talks about his life, his work, motorbikes and losing his mum to cancer when he was still at school.
“You feel like ‘Oh God, I’ve lost my mum!’. You feel like that kid in the supermarket that doesn’t have his mum because he’s gone off to look at toothpaste” He says “That kid’s going ‘What am I without my mum, I’ve always been attached to her and now she’s gone where is she?’.”
Meanwhile in the paediatric area of A&E, teenage parents Connor and Saffron have arrived with their 6-month-old daughter Amira after their GP spotted an irregular heart beat during a routine check up. The paediatric team examine baby Amira while her worried mum and dad look on.
As they wait for news, Saffron talks about how they got together. “I used to stay at the house and in the room there would just be candles and shit everywhere,” she says. “It was a bit cheesy, but it was a bit sweet as well.”
And Connor describes how he found out that Saffron was pregnant. “She sent me a text,” he says. “She put a load of faces on her phone – happy faces, sad faces and question marks – and then she just said ‘I’m pregnant’.”
A teaser for episode eight of ’24 Hours in A&E’
The RTS award-winning documentary series continues from its new home, St George’s in south west London, which has one of Britain’s most advanced and busiest A&E departments. This episode, the last in the series, focuses on the bonds between patients and their family, as well as those between the staff in the A&E department.
Consultant Jai tries to pass on his compassion for patients to his team. “I treat all of my patients as I would treat one of my own,” he says. “I would give them the same amount of care which I would offer to any of my own family.”
Junior doctor Sobi is working with Jai. “Jai is incredibly calm and very patient, he is a good teacher,” she says. “I guess that filters through when you’re working together because it means that things go a lot smoother.”
65-year-old retired builder Roger has fallen four metres from his daughter’s roof while doing some building work for her. The trauma team is concerned that he may have badly injured his head, back and neck in the accident.
Roger’s daughter Lisa heard him fall from her roof ‘like a sack of potatoes’. “The guilt kicks in, thinking he was on my roof,” she says. “You start asking yourself all those questions: ‘What if, what if?’.”
His wife Ellen waits as Roger is taken for a CT scan to find out how badly he’s been hurt. She talks about how Roger has always been a support for her, particularly recently when she lost four sisters.
“He has a sensitive side, very caring; he is always there for me. He used to be a harder a bit fiery. He used to lose his temper if things didn’t go right,” says Ellen. “I seem to hold my emotions in quite a bit, I suppose I have been through too many emotional things in life, I hold them back.”
29-year-old folk musician Tad has come to A&E after developing a dangerously high heart beat. Left untreated it could be very serious and possibly lead to a stroke. Tad has experienced the condition before and knows what to expect. “The best way to describe it would be a rumbling, if you can imagine a train running around your chest,” he says.
Tad’s been treated at St George’s before and is very appreciative of the staff. The doctors try various treatments to get his heartbeat back to normal, but ultimately they have to use an electric shock to try to steady the heart.
Tad talks about his choice of music as a career. “I’ve never been one to follow the flock. Everyone in my immediate family has chosen a career that has absolutely nothing to do with anyone in the family. I’ve taken the same attitude and this is me, this is my pot and I will fit it with whatever I want.”
Meanwhile, 69 year-old Richard is brought to A&E after being found unwell at home by his son, Lee. Doctors are concerned that Richard has developed a very serious infection, possibly sepsis, and begin to treat him with antibiotics.
As doctors try to get Richard’s infection under control, Lee discusses his close bond with his dad and remembers exciting times together when he was growing up. “He was my ‘mad dad’, he used to do things with me my mum would tell him off for. He used to take me to Putney Heath with my air rifle and we used to shoot red bull cans and balloons,” he says.
“He’s my hero, he is my dad. You don’t expect your heroes to get weak,” says Lee. “I’d just to say to my dad, if I could be half the dad you were to me, I’d be a proud man.”
Getting to know Sobi
What is your role within A&E?
I am one of the ED registrars.
How long have you worked at St George’s?
It’s coming up to 18months
How many patients do you treat in an average day? What conditions / illnesses do they have?
I will typically treat between 15-20 patients a day. This will involve people complaining of chest pains, septic patients, traumas and children coming with everyday accidents – so it’s vast and varied.
What did you think when they announced ‘24hrs in A&E’ was going to be filmed at St George’s?
I thought it was a great idea. It gives the public the chance to see the inside workings of the hospital and how closely we work together. It also lets everyone understand the special relationship staff form between each other when working in this kind of environment.
Did you find it had any impact on your day?
To be honest, we are so busy you forget at times the cameras are even there and you just get on with your job.
What have you enjoyed the most from your experience of ‘24hrs in A&E’?
It was wonderful to get an intimate insight into my colleague’s lives and see what they are like outside of work. This gave me a real good insight into what challenges and problems my co-workers deal with.
What is your highlight moment of the series?
It has to be watching and listening to the children’s feedback. This always brings a smile to my face and gives you a totally different insight into what we do here. Family members equally provide some interesting thoughts as well which always helps you appreciate how valued the public make us feel.
What was the biggest challenge you experienced during the filming?
We deal with high-pressure situations all the time, which sometimes involves sad endings. Having a patient’s family and the cameras around during difficult times did make certain situations more difficult. But we have to remember the work we do does not change with our without the cameras.
What is the benefit of St George’s participating in a show like ‘24hrs in A&E’?
It lets the public gain a great fly-on-the-wall perspective of all the important work we do here every day. In addition, it helps the public understand how vital and key our working relationship is – and how this helps us assist all our patients.
What do you think about the reaction to the new series so far?
My friends and family are amazed by the show. They can’t believe how hard we work and the countless cases we deal with. All the feedback I have been given has been very positive and supportive which really puts a big smile on my face.
Is there anything that was or wasn’t caught on camera which you wish wasn’t or was?
Thankfully, none of my cheesy jokes or one-liners were caught on camera or I would have had to hide in shame
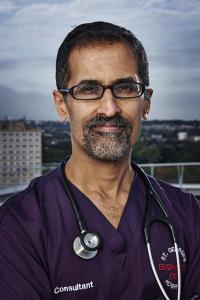
Getting to know Sunil…
What is your role within A&E?
I am one of the Emergency Medicine Consultants at St George’s. As a group our role is to guide and oversee the medical care provided in the Emergency Department at St George’s.
How long have you worked at St George’s?
I have worked in the Emergency Department at St George’s for 3 ½ years.
How many patients do you treat in an average day? What conditions / illnesses do they have?
We treat up to 450 patients a day. We treat the whole range of emergency conditions ranging from the serious and life threatening to those which are less serious. Our expertise is in treating those conditions or illnesses which have developed rapidly and which require emergency treatment.
What did you think when they announced ‘24hrs in A&E’ was going to be filmed at St George’s?
If I’m honest I was a bit apprehensive but I think that was more because I didn’t know what it involved. I had seen the series at King’s and had been impressed but wondered how the staff had felt about being filmed. As I am not particularly media savvy, I think this added to my nervousness.
Did you find it had any impact on your day?
Having to put a microphone on at the beginning of each shift was a bit odd and this initially made me very conscious of what I said but these feelings soon wore off. Also, I was intermittently conscious of the cameras particularly if I saw them moving to point at me!
What have you enjoyed the most from your experience of ‘24hrs in A&E’?
I have really enjoyed seeing my colleagues and the great work they do and also hearing the incredible stories of the patients that we see. Because of the fast and fleeting nature of our work, we often don’t get to fully appreciate our patients’ backgrounds and everything that has brought them to this point. So it’s nice to hear them talk about themselves and their experiences prior to their attendance in the ED.
What is your highlight moment of the series?
I know this sounds a bit self-centred but my highlight has been seeing how the 24 hours in A&E team constructed the episode that I am in. They have been able to take elements of what I said and have wrapped this around patient stories so the over-riding impression reflects the opening title. I think the 24 hours in A&E team are geniuses and are hugely talented in being able to craft episodes like these.
What was the biggest challenge you experienced during the filming?
I initially found it difficult having to explain to patients that we were being filmed and asking whether they minded. This improved over time though, as patients and their relatives said no when they weren’t happy and agreed to the filming when they were so I was satisfied that they had been able to decide freely with the option to say ‘no’ at any point.
What is the benefit of St George’s participating in a show like ‘24hrs in A&E’?
A series like this gives people a more rounded and complete picture of the complexity of clinical work and helps people understand the jobs we do. There are some incredible, highly-skilled and immensely caring individuals who work at St Georges both inside and outside the ED. A series like this acknowledges staff for the clinical care they provide to their patients. The positive effects on staff of this acknowledgement are immeasurable.
What do you think about the reaction to the new series so far?
I think the reaction has been amazing. I am amazed by the response on social media and impressed how staff have handled the attention they have received.
A sneak peek into episode episode six of ’24 Hours in A&E’
In this episode, St George’s A&E team treat two trauma patients who arrive by helicopter on the hospital’s recently opened helipad.
75-year-old Eric has fallen four metres from a ladder while cutting trees in his garden in the rain. He landed on his side, walked into the house and collapsed.
The trauma team stabilise Eric and put him in an induced coma as they get a CT scan to discover his internal injuries. Margaret, Eric’s wife of fifty years arrives with their sons and grandson to be with him.
“I kept telling myself ‘everything will be OK’,” says Margaret. “I knew I couldn’t start getting too bad because then they’d all start crying so I had to sort of keep myself composed.”
Eric’s a shoemaker who’s even made riding boots for the Queen. “That’s as high as you can go,” says a proud Margaret.
29-year-old IT consultant Mihhail is airlifted to St George’s after crashing his motorcycle into a bollard at high speed. He’s taken straight for a CT scan to look for hidden injuries.
Doctors are concerned that he has very serious internal injuries, including a lasceration to his liver and order a code red, an emergency blood transfusion due to the level of internal blood loss. He’s transferred to the Intensive Care Unit while specialists decide how to repair the damage to his liver and how best to stop his internal bleeding.
Mihhail’s girlfriend Joanne arrives to be with him. They met through her father, who’s also a biker. She explains why that day felt different from the start. “That was the only day I didn’t say to him ‘ride safe’,” says Joanne. “If I’d said it I think he would have been OK.”
Meanwhile, 22-year old performing arts student Maria is complaining of chest pains. She has a complicated condition meaning that she suffers from pain every day, affecting her sleep and mobility. “For someone as active as I am, with so many dreams and aspirations, it’s very hard to suddenly find that your body’s a prison,” she says.
And Rusty (age?) has been hit by a car while crossing the road to deliver a newspaper to a friend and has a badly broken ankle. Consultant Will is treating the self-confessed life-long lady’s man.
“There’s never been any deliberate pattern to my life, it’s all happened by sheer coincidence,” says Rusty. “I am so determined to get well, to move ahead. Who knows what ‘ahead’ is. I’m not going to close shop, not yet!”
Work and play in episode five of ’24 Hours in A&E’
In this episode, the team at St George’s treat patients who’ve injured themselves through work or play.
60-year-old Iain is rushed in by ambulance after falling ten feet off a ladder onto his head while fixing an air-conditioning unit at work. He has a deep laceration above his right eye and can’t see through it. Doctors can’t guarantee that he won’t lose sight in his eye.
Consultant James is leading Iain’s treatment. “Bad eye injuries are surprisingly rare,” says James. “The eye is quite protected. If you get hit by something flat, your eye is spared.”
While the trauma team fights to save the sight in Iain’s eye with the help of the hospital’s opthamologists, Iain’s wife Loraine and daughter Leanne wait nervously by his side.
Loraine discusses their special bond. “He’s my soul mate as well as my husband and my best friend,” says Loraine “We’re always together. When we go to bed in the evening we always go up the stairs together.”
20-year-old student teacher Lloyd is helped into A&E by his friend Mollie after injuring his foot on an inflatable obstacle course on their last day at university. Medics fear that swelling is stopping blood circulating in Lloyd’s foot, which could be serious and may need surgery. Luckily Mollie is by Lloyd’s side supporting him as she has done through other tough times at college.
Meanwhile, 13-year-old Lucy has fallen off the trampoline in her family’s garden, getting trapped in the springs and hitting her head on the ground. When dad Tim got to her she was losing the feeling in her feet and hands. Doctors are worried that she may have a neck injury.
Getting to know Daryl…
Daryl is one of our senior charge nurses. He is seen caring for 22-year-old Paul, a stabbing victim who features in episode four of ’24 Hours in A&E’ (aired 20/11/14).
What is your role withing A&E?
I am one of the Senior Charge Nurses in the department, I manage a team of nurses in their development as well as the day to day running of shifts when I am in charge.
How long have you (or did you) worked at St George’s?
I’ve worked at St George’s for 4 years.
How many patients do you treat in an average day? What conditions / illnesses do they have?
We see around 350-400 patients everyday with a massive range of injuries and illnesses, it’s very unpredictable.
What did you think when they announced ‘24hrs in A&E’ was going to be filmed at St George’s?
When I first heard that ’24 hours’ would be filming in the department I was slightly apprehensive. I was unsure we would be able to add anything new to the show since Kings did such a great job in their time.
Did you find it had any impact on your day?
The filming didn’t really have an impact on my day, it’s always busy and there’s always something going on so we all just got on with our jobs, wearing a microphone and seeing the cameras just became part of the routine.
What have you enjoyed the most from your experience of ‘24hrs in A&E’?
Going up to the helipad to have the publicity shots done was probably the highlight since staff aren’t allowed to go up there in normal circumstances. It was a really sunny day and you could see the whole of London.
What is your highlight moment of the series?
I’ll have to wait to the end of the series to say!
What was the biggest challenge you experienced during the filming?
I found it all quite easy going.
What is the benefit of St George’s participating in a show like ‘24hrs in A&E’?
It will showcase the variety in our day to day shifts and show what an amazing team we have in the department.
What do you think about the reaction to the new series so far?
As far as I can tell its all been positive so far, hopefully that will continue, my wife and daughter are certainly enjoying it.
Is there anything that was or wasn’t caught on camera which you wish wasn’t or was?
I think there will always be cases that were really interesting but consent was an issue or the patient was in an area where there wasn’t a camerabut I think the ’24 hours’ team did a great job at capturing us all at work.
Spoiler alert for episode four of ’24 Hours in A&E’
In this week’s episode those providing the bedside support take centre stage as a girlfriend, a wife and a daughter keep spirits high in difficult times.
First up is 22-year-old Paul who’s been stabbed in the face and arm with a broken bottle outside a nightclub in Kingston. The former boxer is rushed into A&E accompanied by his girlfriend Naveena.
Staff at St George’s are used to dealing with stabbings and charge nurse Daryl explains what they’re looking out for. “The main concerns are going to be scarring, loss of vision if they’ve done something to their eye,” he says. “Someone could die from a facial stabbing: your spinal cord runs right down the back of your neck, the base of your skull and your brain.”
As the medical team works to stop the bleeding and treat Paul’s wounds, his girlfriend reflects on his sensitive side. “Paul is very good in situations that I’m not so good in,” says Naveena. “Violent things or things where he knows that something wrong’s happening. He’s always very protective, nothing ever goes wrong.”
70-year-old John arrives with his wife Francesca after falling awkwardly while out running and painfully dislocating his shoulder. To get John’s pain under control quickly the medical team give him Ketamine and the hallucinogenic side effects keep Francesca and the staff entertained as they prepare to relocate his shoulder.
While doctors notice a loss of sensation in John’s arm and treat him for potential nerve damage, his wife Francesca talks about how they met and their life together.
“When I met him he used to rally a little Mini,” she says. “I said to mum ‘Oh, he’s a really nice guy. He’s just such a nice chap. But John was going out with somebody, which I didn’t know. And she was his navigator. So I suspect he might have asked me out before he told her!”
Meanwhile 93-year-old Angela is brought to A&E by her daughter Elizabeth after suffering from blood loss and disorientation at her care home. While doctors investigate what is causing Angela’s symptoms, Elizabeth keeps her company and shares happy memories of growing up.
“We were all born very close together. Three daughters with a really lovely mum,” she says. “We used to fight over sitting on her lap. You might find her sitting at the breakfast table with all three children sort of hanging from her just wanting to be around her.”
Getting to know Sandra…
What is your role within A&E?
My role is staff nurse in A&E dept.
How long have you worked at St George’s?
I have worked at St. Georges over four years, two years medical assessment unit (MAU) and two years A&E.
Why did you decide to become a nurse?
I became a nurse after I lost my eldest son in a car accident.
How many patients do you treat in an average day? What conditions / illnesses do they have?
We see hundreds of patients on a daily basis.
What did you think when they announced ‘24hrs in A&E’ was going to be filmed at St George’s?
I was very wary when I knew 24 hours cameras were coming in, my biggest fear was professionalism, confidentiality and dignity, from a patient point of view.
Did you find it had any impact on your day?
At first I was very unsure of cameras, but soon forgot they were here and carried on as normal. In fact sometimes I forgot the microphone was on and went to the loo to spend a penny. I cringe at them listening to me tiddle in the gallery!
What have you enjoyed the most from your experience of ‘24hrs in A&E’?
The 24 hours team seemed to blend into the background and seem to be part of the team too. They were very polite and not at all intruding.
What is your highlight moment of the series?
I think seeing our department in the first episode on TV was great! It portrayed just how strong and professional our team is.
What was the biggest challenge you experienced during the filming?
The biggest challenge was doing the interview on camera. It was a weird experience! I nearly didn’t do it, I usually don’t like even like having a photograph being taken. I am very camera shy.
What is the benefit of St George’s participating in a show like ‘24hrs in A&E’?
St George’s will benefit from the series as it will show that we are a great team, and how hard it is working within the NHS, but also it can be so very rewarding.
Is there anything that was or wasn’t caught on camera which you wish wasn’t or was?
I looked after a young man who fell off a zip wire, he totally lost his memory and was chatting about seeing his grandfather in the ambulance. Suddenly he burst into tears as he said he had just remembered his granddad had died a few years ago.
We were looking after him and his sister started to get tearful when she saw me, and said I looked like their mum who died. She had brought her brother up and looked after him as a child.
I had to hide in another cubicle because they moved me to tears. I wondered whether he really did see his granddad, was he looking after him in the ambulance? Sadly this was not caught on camera, but I will never forget this young man.
Weeks later I received a card saying he still does not remember what happened that night in A&E but he remembered me so well, and how grateful he was for my care, I cried again!
A sneak peek into episode three of ’24 Hours in A&E’
Filmed around the clock by 104 cameras, the series captures dramatic and emotional stories of love, life and loss on the frontline of the NHS. This week’s programme focuses on the support given to patients by their loved ones and staff reflect on personal stories that inspired them to work in A&E.
38-year-old tree surgeon, Paul is rushed into Resus by ambulance from Kent after falling 25 feet from a tree when his harness failed, hitting his head on a concrete pole as he landed. Paul has a head wound and is complaining of shooting pains in his back as well as pins and needles in his feet.
Doctors are immediately concerned that he may have injured his spine. “When somebody falls you worry about the head, then you worry about spinal injuries. When the patient comes in if they’re complaining of pins and needles my heart always sinks,” says orthopaedic doctor Mike. “It could be a sign that there is trauma to the spinal cord which can cause paralysis.”
A CT scan confirms that Paul has broken a vertebra in his back and medics are concerned fragments of bone could damage his spinal cord.
Paul’s wife Emma realised things were serious when she was told Paul had been taken to St George’s rather than their local hospital. “You think ‘What if he doesn’t walk again?’,” she says. “It’s horrible to see somebody that you look upon as big and strong and seeing them just going insane with the amount of pain they’re in. I just felt pretty helpless, but all I could do was hold his hand.”
Meanwhile 66-year-old Anthony, who has recently been diagnosed with Parkinson’s and Prostate cancer, has fallen down fifteen stairs at home. He is very frail and a scan reveals that Anthony has broken some ribs, puncturing a lung and will need a chest drain.
His wife Jennifer waits and reflects on how the couple met through a dating agency in 1975. “We met up in London somewhere. And he had this funny tweed coat with a belt round the middle and I thought ‘I don’t like that!’,” says Jennifer. “I don’t know what happened to the coat, but he’s lovely. He’s my soul mate.”
Nurse practitioner Becky and nurse Sandra reflect on what inspired them to work in A&E.
“I think a lot of people go into nursing because something happened to them when they’re younger,” says Becky. “My mum died of cancer when I was 8 and anything I can do to stop anyone else go through that kind of terrible emotion of losing someone, that’s why I wanted to be a nurse. The thing about working in A&E is that a lot of really horrible things happen to really good people…it makes you grateful for what you have.”
“People assume I’ve been nursing all my life, but it’s only been the last couple of years,” says Sandra. “I was a lorry driver and a bus driver, then a pub manager and now I’m a nurse. I had a son that was involved in a car accident, I lost him. So instead of curling up and going into a little ball I decided to get myself off to college, get an education and put myself into that. I always wanted to be an A&E nurse. I like to help others that are going through what I went through. That’s how I help myself.”
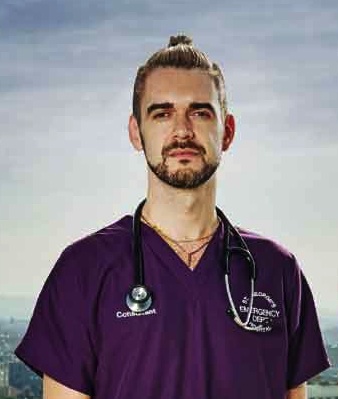
Getting to know Will…
Will is an emergency medicine consultant at St George’s Hospital. He is seen in episode two of the 7th series of ’24 hours in A&E’ (aired 06/11/14) treating 19-year-old Billy who has been thrown twenty feet from his motocross bike during a race.
What is your role within A&E?
I am a Consultant of Emergency Medicine and Pre-Hospital care with a both a clinical and teaching role.
How long have you worked at St George’s?
I have worked at St. George’s since April 2012.
How many patients do you treat in an average day? What conditions / illnesses do they have?
We treat approximately 380-390 patients both adult and paediatric per day, ranging from minor illness and injuries to major trauma and cardiac arrests.
What did you think when they announced ‘24hrs in A&E’ was going to be filmed at St George’s?
I was very excited about the project and would be a great opportunity for the Trust to show what amazing work the team performs on a daily basis 24 hours a day, 365 days of the year.
Did you find it had any impact on your day?
The filming process had very little impact on our day to day work – the cameras were very soon forgotten and genuine natural work was captured.
What have you enjoyed the most from your experience of ‘24hrs in A&E’?
I have enjoyed the positive feedback about our department from the first episode – a real boost to the team.
What is your highlight moment of the series?
The high quality care in an empathic manner we deliver to our patients.
What was the biggest challenge you experienced during the filming?
I greatest challenge was consenting and informing patients to the series. The delicate balance of ensuring no pressure is put on them to be involved and that it is their care is the most important thing.
What is the benefit of St George’s participating in a show like ‘24hrs in A&E’?
We, as a whole Trust, should be very proud of the healthcare we deliver – all day, every day.
What do you think about the reaction to the new series so far?
Only positive.
Getting to know Mo…
Mo is a trauma registrar who stars in episode one of the 7th series (aired 30/10/14) removing an embedded needle from a patient’s foot.
What is your role within A&E?
As a trauma registrar you must be present at all major trauma calls and lead the assessment and management of the unwell patient in conjunction with the emergency department consultant. We also provide a specialist service for all trauma and orthopaedic issues (including foreign bodies in the foot!)
How many patients do you treat in an average day? What conditions / illnesses do they have?
Obviously this ranges, but on average we can deal with up to five or six major trauma calls in any 12 hour shift. These patients will have suffered “polytrauma” (meaning multiple injuries) and therefore may have head, chest, abdominal, pelvic and limb injuries. We lead patient care and coordinate with other specialities when their input is also required.
We may also admit another similar number with relatively less severe injuries, such as hip, spine or limb fractures, and we may review many more and discharge them from A&E. We also support the entire hospital’s inpatients, and its partner hospitals for tertiary centre advice, as well as local GPs.
What did you think when they announced ’24 Hours in A&E’ was going to be filmed at St George’s?
I was anxiously excited but what a great opportunity for the hospital to showcase the fantastic job it does treating its patients.
Did you find it had any impact on your day?
No. Well, at first I felt the cameras presence, but that soon disappeared.
What have you enjoyed the most from your experience of ’24 Hours in A&E’?
The love and support that has been shown!
What is your highlight moment of the series?
I haven’t seen it all yet so I’m looking forward to finding out!
What was the biggest challenge you experienced during the filming?
Everyone warned me off not being involved… Apparently at best you could come off looking normal. I’m glad I had the courage to engage with the fantastic production team.
What do you think about the reaction to the new series and your part in it?
I’ve been massively overwhelmed.
What is the benefit of St George’s participating in a show like ’24 Hours in A&E’?
It’s a first class hospital and people should see that. I hope it does the hospital a great deal of positive publicity so it can secure its services and make the transition to a foundation trust.
Is there anything that was or wasn’t caught on camera which you wish wasn’t or was?
There was a young polytrauma patient involved in a high speed head on collision that had numerous severe injuries including an open chest wound, intrabdominal injuries and a fracture dislocation of his hip. I washed out his thoracic wall/cavity, put a chest tube in and reduced his hip dislocation. This would have made great TV, but more importantly I would have loved to see his progress as we had to transfer him to King’s for his liver injuries.
A teaser for episode two of ’24 Hours in A&E’
The RTS award-winning documentary series continues at its new home, St George’s Hospital in south west London, which is home to one of Britain’s most advanced and busiest A&E departments.
Filmed around the clock by 104 cameras, the series captures dramatic and emotional stories of love, life and loss on the frontline of the NHS.
This week’s programme focuses on the treatment of men who’ve been injured on two wheels.
19-year-old Billy has been thrown twenty feet from his motocross bike during a race, suffering multiple spinal injuries and he’s lost sensation from the chest down. He’s been transferred from a hospital in Brighton to St George’s for treatment by the specialist neurosurgical team.
“Whenever we have a potential spinal injury patient coming in, you realise that’s a real time-critical injury,” says consultant Will. “If they have paralysis, we have to diagnose why they have it and see if there’s something that we can reverse. But unfortunately, with spinal injuries there is a higher possibility that this won’t get better.”
Billy’s parents and brothers witnessed his crash and are by his bedside, braced for the worst. “I’ve got three boys, they love fast sports. I didn’t discourage them from doing what they wanted to do. The main thing I didn’t want my boys to do was to ride a motorbike out on the road, “says Billy’s dad, Brad. “I just didn’t believe it, it’s as if they’re talking about someone else. You don’t ever expect it to happen, not to yours.”
Meanwhile 53-year-old teacher Dave has facial injuries after riding his new bicycle into the back of a stationary car in Richmond Park. His wife Kate received a phone call shortly after the accident. “It was his friend Bugsy, who he’d been cycling with. He said ‘There’s been an accident, he’s come off the bike and an ambulance is on its way’,” says Kate. “It was when he said ‘He’s lost part of his face and we’ve got it on ice’, that scared me a lot.” The crash is a wake up call for Dave. “What dawns on you is that you’ve absolutely no control over the situation at all,” he says. “That makes you a little more philosophical and it makes you realise you are quite vulnerable really. I should take life a little more easy, maybe I’ll go back to golf and fishing!”
And 30-year-old adrenaline junkie and ex-Royal Marine Richard has badly dislocated his thumb after falling off a bicycle. As the emergency team try to realign the tip of his thumb, Richard enjoys the effects of the pain-killing gas and air while reflecting on his time in the marines and the evolutionary benefits of risk.
Consultant Will talks about how risks are part of normal life. “There are calculated risks that we take. Most of the time you get away with it, you learn from it,” he says. “But every so often when you challenge yourself, you fall short.”
Getting to know Louise…

Louise Halfpenny is the head of communications for St George’s Healthcare NHS Trust. She was instrumental in securing St George’s as the new home for ’24 Hours in A&E’.
Why did the trust agree to be filmed for the series?
We thought it would be a great way to show the public what really goes on behind the scenes of a busy emergency department. We’re proud of our staff and what they achieve. You’d have to be -there’s no hiding place with more than 100 cameras in place!
How much was the trust paid for being part of the series?
We were given a facility fee for taking part.
Where will the revenue go?
Some of it was used for additional staff time needed to make the show happen and some will be used to begin much-needed improvements to our intranet.
Were staff paid for participating in the series?
No, not directly. When we needed staff to spend time to help with the programme then money was used to backfill them so that patient care was not affected.
Did all patients give their consent to be filmed for the series?
Yes. Absolutely!
How did you know that patients were able to give consent?
Before filming started the trust carefully considered the consent process. Our medical director, information governance leads and our legal team looked through the production team’s processes very carefully and were happy with their approach. A contract was then signed. In addition, we spoke to colleagues at King’s where the series had been filmed previously. Their experience gave us even greater assurance about consent.
How much disruption did the filming cause for patients?
Hardly any. There were only a couple of members of the production team in the hospital at any one time. The cameras are installed so there weren’t lots of people filming patients. The cameras were operated remotely.”
How did you make sure patients, visitor and staff were kept safe during filming?
The cameras and cabling were installed when the emergency department was at its quietest. Our own estates team played an important role in overseeing this – often at very unsociable hours. We also organised a briefing for more than 100 staff from The Garden Productions to tell them about safety, conduct and infection control measures before filming started. We’re grateful to The Garden Productions and our estates staff for doing all they could to minimise disruption and put safety first.
Wasn’t it distracting for doctors/nurses to be filmed while treating patients?
Staff are focused on treating patients first and foremost. Everyone soon got used to them. Some staff, patients and their visitors also wore mics but only if they were completely happy to do so.
Was it really necessary to show such graphic scenes of injuries?
The programme is broadcast after 9pm and its title suggests what might be included. Serious injuries are part of everyday life in a major trauma centre like the one at St George’s. Many of the more gruesome shots have been edited out but it was important to leave in footage that formed an important part of the patient’s story.
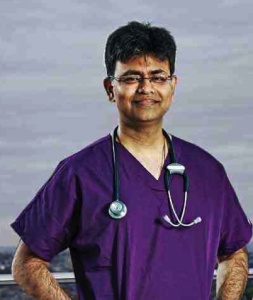
Getting to know Jai…
Jai is a trauma consultant at St George’s Hospital. He is seen in episode one of the 7th series of ’24 hours in A&E’ (aired 30/10/14) treating a young woman called Kerry who has lost part of her leg in a motorbike accident.
What is your role within A&E?
Care Group Lead & Consultant Adult and Paediatric Emergency Physician
How long have you worked at St George’s?
5 years and 11 months
How many patients do you treat in an average day? What conditions / illnesses do they have?
The department receives approximately 350 new patients a day. When I am on a clinical shift, I normally work a 9.5 hour shift. The number of patients I see depends on the area I work. For example, resus work would involve seeing less number of patients compared to majors or in urgent care as resus patients are more sick. However, on an average I would see approximately 20 patients per shift. I encounter different patients depending on the location I work. For example in resus patients present with major trauma, cardiac arrest, sepsis, chest pain, difficulty in breathing, dislocation of joints / fractures, whereas in urgent care patients present with minor injuries and minor illnesses. I also receive and treat children presenting with various illnesses and injuries.
What did you think when they announced ‘24hrs in A&E’ was going to be filmed at St George’s?
I was involved with the ‘24hrs A&E’ project at the very beginning and showed eagerness and enthusiasm which enabled St Georges to reach the final shortlist. The Clinical Director Dr Phil Moss and Clinical Director for Major Trauma Dr Heather Jarman helped the ED secure the project.
Did you find it had any impact on your day?
At the outset, the filming I felt did have a slight impact on most of the staff including myself. We were a bit anxious as we felt the presence of cameras a bit voyeuristic and wanted to ensure that we came across well and represented the department and the trust in good light. However, after a couple of weeks we naturally slid into our normal working style as our work normally encapsulates and reflects our trust values of being Kind, Excellent, Responsible and Respectful.
What have you enjoyed the most from your experience of ‘24hrs in A&E’?
I have enjoyed and learnt from watching “ER” series when I was growing up and the ER music still echoes in my head whenever I walk into the resus room. I had a secret desire to appear on a TV show. 24 Hours A&E made it possible on two counts; I appear in their initial episodes as well in their pre-title sequence. There are a lot of good learning points in the programme both for the public and doctors alike. I hope this series will prove to be as informative and appealing as ER was to me!
What is your highlight moment of the series?
I have not watched all of the scenes that have been filmed so far to know which the highlight of the series is. However, Series 7 kicks off with a young female who was involved in a major trauma (amputated her leg and fractured her thigh). Receiving and treating her from an out of area helicopter emergency crew would be my highlight as I was involved and wanted to do the best for her as she reminded me of my elder daughter who was only a few years younger to her.
What was the biggest challenge you experienced during the filming?
The biggest challenge I faced during filming was to keep my banter with my ED staff under check. I am known to be cheeky!
What is the benefit of St George’s participating in a show like ‘24hrs in A&E’?
The benefit of St Georges participating in a show like 24hrs in A&E is to show to the world what an Awesome and Audacious A&E team, St Georges possesses. We are seen to be Effective, Efficient and most of all Caring!!
Is there anything that was or wasn’t caught on camera which you wish wasn’t or was?
There are number excellent colleagues from various sections of the department and from the rest of the Hospital who were caught on camera during the filming, some of us more so than others. However, what I want to emphasise is the greatness of the ED team does not only belong to those who appear on the TV screen but to every member of the department and hospital team who work tirelessly every day to deliver the best possible care for the patients coming into St George’s ED. Every member of such a large team could not be adequately captured on camera. However, I am ever so grateful to be part of such an awesome team!
Episode One – 30th October 2014 9pm
Channel 4’s award-winning series, 24 hours in A&E spent six series and seventy episodes at King’s College Hospital in south London, but now the new series will feature St George’s Hospital in south west London, whose A&E department is one of the most advanced and busiest in the world.
In the first episode of the new series, St George’s trauma team fight to save the life of a young woman after a horrific motorbike accident.
29-year-old dental nurse Kerry arrives from Essex by emergency air ambulance on the hospital’s new helipad as a ‘code red’ patient. She was riding her motorbike when she lost control and crashed, completely severing her right leg below the knee.
Kerry’s grandparents, Dennis and Angie, received a phone call about the accident and were among the first people on the scene. “We got there and saw Kerry laying in the ditch,” says Dennis. “I see these two fellas running up and down the road. They didn’t know who I was and I said ‘Excuse me, what are you looking for?’ and he said ‘We’re looking for the young girl’s leg’.”
Due to the severity of her injuries, specialists from seven different departments have been called in to treat Kerry. Trauma consultant Jai is in charge. “When you say ‘code red’, you get a patient who’s lost a lot of blood and they are critically unwell,” he says. “If you cut off your lower limb, the worst thing that can happen is that they can lose the whole volume of blood and as a result your heart goes into cardiac arrest.”
But the medics need to stabilise Kerry before they can send her for a CT scan to see if it’s possible to re-attach her leg. “Time is very critical when we are considering re-attachment of the leg,” says consultant Jai. “But the first priority is always life. Limb comes second after life.”
Kerry’s grandparents have always been worried sick about her getting a motorbike. “We literally begged her not to, but Kerry desperately wanted a motorbike, so she went out and got one,” says Dennis. “Our heart was in our mouth every time she went out on that bike until I heard that motorbike come back here.”
Meanwhile 11-year-old Luke is brought into the department after suffering a prolonged epileptic seizure. Luke has a form of complex epilepsy that has left him with severe learning difficulties. He has up to three seizures a week.
While the paediatric team stabilises Luke, his mum and dad discuss their love for him and the challenges of living with Luke’s condition.
“Do I resent my son’s illness? No, absolutely not. Do I become jealous of parents who have ‘normal’ children? Without a doubt,” says Luke’s dad, Jack. “You’re different from other people, that’s the way it’s going to be, it’ll probably be that way for the rest of your life…it’s not even clear if he’s going to outlast me or I’m going to outlast him.”
But there are pluses too. “We went through such a horrific time when he was little, but you come out the other end and you realise ‘OK, this is different than what I was expecting, but actually not awful, it’s actually very valuable and very positive’,” says Luke’s mum, Catherine. “He’s such a delight, he’s so positive, he’s so much fun, he’s got a healthy stubbornness about himself – we’d like to wrap him in cotton wool and he refuses to let us do that.”
And 19-year-old Tina comes to A&E after stepping on a sewing needle which is stuck inside her foot. But she seems more keen on taking advice from her mum in Lithuania than from Mo, the doctor treating her.