Services
St George’s University Hospitals NHS Foundation Trust is one of London’s leading teaching hospitals with an international reputation for quality of care and cutting-edge treatment. In this area you will find detailed information on all the services we provide. We provide services to both children and adults.
Need to change or cancel your outpatient appointment? You can change or cancel your appointment at St George’s Hospital online via our appointment amendment form.
Filter services
Site
Service
D

Diabetes and endocrinology
Our Diabetes and Endocrinology departments, located at St George’s Hospital, Queen Mary’s Hospital, and St John’s Therapy Centre, specialise in managing diabetes and hormonal disorders.
G

Gastroenterology
Our Gastroenterology and Hepatology Department teams specialise in diagnosing and treating conditions of the gastrointestinal tract, liver, pancreas, and biliary system.

Genomics - South West Thames Centre for Genomics
The South West Thames Centre for Genomics at St George’s offers specialised genetic services, including diagnostics and counselling, to patients in South West London, Surrey, and West Sussex. Our UKAS accredited laboratory provides diagnostic analysis and reporting for genetic disorders.

Gynaecology
The Gynaecology service at St George’s and Queen Mary’s Hospitals provides expert care for women’s reproductive health, including diagnosis and treatment of various conditions.
M

Maternity
St George’s Maternity Unit offers comprehensive care during pregnancy, birth, and postpartum. We recommend completing an online self-referral form by 7 weeks of pregnancy to schedule your midwife appointment.
N
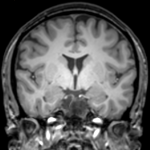
Neurosciences Centre
The Atkinson Morley Regional Neurosciences Centre at St George’s Hospital offers internationally recognised care for neurological conditions, including neurology, neurosurgery, neurorehabilitation, and stroke services. Our comprehensive services cover diagnosis, treatment, and care for disorders of the brain, spinal cord, and nervous system.
O

Orthotics service
The Orthotic Clinical Service aims to provide a comprehensive inpatient and outpatient orthotic service to aid movement, correct deformity and relieve discomfort. The team specialises in complex rehabilitation problems for patients with musculoskeletal, degenerative and/or neuromuscular problems; many of which utilise our large range of multidisciplinary teams.
R

Rehabilitation services
Our Rehabilitation Service at Douglas Bader Rehabilitation Centre offers specialised care, including prosthetics. The Gait Lab offers detailed walking analysis and functional electrical stimulation (FES) to support neuro-rehabilitation, orthopaedic surgery, and more.
S

Stop smoking service
We encourage those admitted to the hospital to seek support for quitting or temporary abstinence through nicotine replacement therapy, with the hospital’s stop smoking service offering advice and support during and after your stay.

