Induction of Labour
On this page:
This page explains the induction of labour (IOL or ‘induction’) process for those who are advised to have labour started artificially. If you have any further questions, please speak to the doctor or midwife caring for you.
Why might I be advised to have an induction?
Mostly, labour starts naturally before 42 weeks, but around 1 in 3 people will be advised to have an induction of labour at St George’s for various reasons which include:
- Your pregnancy has lasted over 41 weeks (called ‘Post Dates’)
- Your baby is not growing as it is supposed to or is showing other signs of not doing well inside the womb
- You have a medical condition such as high blood pressure or diabetes
- You are over 40 years old or over
- You have been assessed as high risk ASPRE – this means there is a higher chance of high blood pressure, pre-eclampsia and/or issues with your placental function that can sometimes affect baby’s growth
- You have experienced reduced fetal movements at term (from 40 weeks)
- Your waters have broken, but your labour has not started within 24 hours. (There is a small increased risk of infection to you and baby 24 hours after they have broken, so we offer induction if labour has not started and monitor you both carefully)
- Your waters have broken before labour and the baby has done a poo, usually called ‘meconium’ (we would advise IOL as soon as possible in this instance as there are increased risks to your baby).
If we recommend an induction of labour, the reason will be explained, and you will have an opportunity to ask questions. It is always your decision, and the team will outline the risks and benefits to you and baby. If you choose not to have an induction, you may be referred to our Birth Options clinic or to a more senior doctor so they can give you further information to make an informed decision and a care plan can be created with you.
Why do you offer induction for pregnancies that go beyond 41 weeks?
If you have an uncomplicated pregnancy and labour has not started by 41 weeks, local and national evidence supports having an induction from 41 weeks with the aim of delivering your baby before 42 weeks. This is to avoid an increased chance of caesarean birth, baby being admitted to the neonatal unit, and stillbirth (baby dying before birth). This aligns with The National Institute of Clinical Excellence (NICE, 2021) guidelines, and World Health Organisation (WHO) recommendations. We understand the topic of stillbirth is a sensitive issue for all expectant parents. Here we touch on some information for you to make a fully informed decision about an induction.
A recent large review of data looked at pregnancy, labour, and birth outcomes when labour was induced compared to when labour was not induced before reaching 42 (or more) weeks. This data compares pregnancies at low risk for complications, therefore if you have complexities where we recommend induction earlier than 41 weeks, please discuss your individual risks with your midwife or doctor.
The table below demonstrates a comparison of different outcomes in any low-risk pregnancy that may be of interest when comparing induction with no induction. If you don’t understand these figures, please ask a healthcare professional to help you.
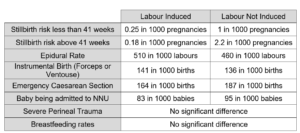
Middleton P, Shepherd E, Morris J, Crowther CA, Gomersall JC. Induction of labour at or beyond 37 weeks’ gestation. Cochrane Database of Systematic Reviews 2020, Issue 7.
Is there anything I can do before being induced to help labour start?
A Membrane Sweep
Your midwife will offer you a membrane sweep (a ‘stretch and sweep’ or ‘sweep’) from 39 weeks. This is always an individual choice and will not affect your care pathway if you choose not to have it. A membrane sweep is not a formal method of induction of labour, and it can take place during your midwife appointments. There may be some instances where a sweep is not recommended or should be done with caution. Please discuss with your Midwife or Doctor whether a sweep is suitable for you and your pregnancy.
There is some evidence that a sweep can trigger the production of natural labour hormones – evidence suggests there is a 20% increased likelihood of going into spontaneous labour 2-3 days after a membrane sweep compared to those who have not had a sweep, but it does not improve the likelihood of an unassisted vaginal birth. It is safe to have up to 3 sweeps in a pregnancy, but they must be at least 72 hours apart.
It is a procedure that some say feels like a smear test which is likely to be uncomfortable, in which a healthcare professional places 1-2 gloved fingers into your vagina to reach just inside your cervix (neck of the womb) and make a sweeping circular movement to separate the membranes (sack around the baby) from the cervix.
Normal symptoms after a sweep include pink/mucous discharge, abdominal cramping, very light spotting of blood from your vagina (this should go away quickly).
If you are concerned that the bleeding is not reducing or is getting worse, you think you are in labour or have any other concerns, please call the Maternity Helpline – 0208 725 2777.
What types of induction of labour are there?
The method/s of induction that will be recommended to you will depend on multiple factors in your pregnancy and medical history. These include:
- A vaginal prostaglandin pessary (Propess or Prostin)
- Dilapan (hydrogel gel rods that can open your cervix enough to break your waters)
- Artificial rupture of membranes (breaking your waters) or ‘A.R.M’
- Syntocinon drip through a tube inserted in your vein (oxytocin hormone drip)
- Cervical balloon catheter
It is common for a combination of methods to be used to bring on established labour, sometimes taking 2-3 days to achieve the regular contractions needed to birth your baby. At any time during the process, you can discuss further steps with a senior midwife or obstetrician. Please see below for an explanation of all methods.
Can I choose where to have my baby with an induction?
When you have an induction of labour, local and national guidance advises having your baby in a setting led by obstetric doctors such as the St George’s Delivery Suite. This is because when any sort of hormonal method like a pessary or oxytocin drip is in use, you are advised to have your baby’s heartbeat monitored continuously from when established labour starts, until the birth.
There are some scenarios where you can have your baby in a midwife led setting such as the Carmen Birth Centre if labour establishes with one vaginal prostaglandin pessary, however in this setting, the baby’s heartbeat is monitored in a different way that is not continuous.
If you would like to consider using the Carmen Birth Centre during your induction, more detailed discussions must take place with a senior midwife during pregnancy to explain the difference in types of baby monitoring, and you must have a full understanding of the risks and benefits of both settings to you and baby to make your choice.
What is a Vaginal Prostaglandin Pessary?
The two types of vaginal prostaglandin pessary used at St George’s are Propess and Prostin. Propess is the most common method. Its purpose is to soften or ‘ripen’ your cervix, make your body’s hormone receptors more ready for labour, and for some people, may help contractions to start.
Propess looks like a small tampon that is inserted into the upper part of your vagina by a midwife or a doctor during an internal vaginal examination which can be uncomfortable. The string sometimes sits in the opening or just outside of the vagina which is normal.
Propess can be used for inductions on the Antenatal Ward or Delivery Suite, or in the Day Assessment Unit if you are suitable to have an ‘Outpatient Induction of Labour’ (see the ‘Outpatient Induction’ section below).
Before it is given, you will have a full assessment and discussion with a midwife, baby’s heartbeat will be monitored for about 30 minutes using a CTG (cardiotocography) machine, and you will have a discussion with a doctor. After it is inserted, baby’s heartbeat will be monitored for a further 30 minutes. We will then encourage you to walk around and eat/drink as normal. Your midwife or doctor will discuss how often we plan to check on baby using a CTG monitor throughout the process. Please tell us immediately if you have any concerns about your baby’s movements during the induction.
After the Propess is inserted, it is likely you will experience some mild abdominal cramping, but it may take a considerable length of time, and often further induction methods before labour starts, sometimes 2-3 days. This is normal and often the expected amount of time for a successful induction. The Propess will stay in for up to 24 hours and will be removed by pulling the string (like taking out a tampon). Sometimes we will recommend a second Propess for another 24 hours if your cervix has not made enough changes.
In some circumstances, we may advise Prostin, which is the other form of vaginal prostaglandin pessary and will be discussed with you in more detail if the doctor on duty feels it will benefit you. It is a white tablet inserted the same way as a Propess. The tablet dissolves and absorbs in the vagina and an assessment will be advised 6 hours after it is inserted.
Before you are given the Propess, your baby will be monitored on a CTG machine for about 30 minutes. Once the propess has been inserted, your baby will be monitored again for a further 60 minutes. After this, you can walk around as much as you want.
After the Propess is inserted, your labour may start straight away, or it may take several days before your baby is born. Both of these reactions are normal as everyone reacts differently to the induction process. The midwives will keep your informed of your progress and offer advice and support. The Propess will remain inside you for up to 24 hours, before being removed easily by pulling on the string. Sometimes a further Propess is advised to help continue the induction process.
The other hormonal option is Prostin. This is only used in special circumstances after a discussion with the doctor on duty. If this is an option for you, your doctor will discuss this in more detail. It is the same medication as Propess but is given for 6 hours and absorbs itself as it softens the cervix.
What is Dilapan?
Dilapan can be offered in any pregnancy apart from those with known Group B Strep or bacterial vaginosis infection. DILAPAN-S® are made from a patented hydrogel material called Aquacryl which come in the form of small matchstick-sized rods.
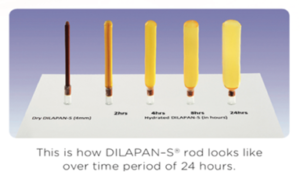
It is different from the other induction methods as it slowly readies the cervix for labour by mechanical means rather than through using any hormone-based medications, however there is a 10% higher chance of you needing Syntocinon with Dilapan compared to Propess due to the lack of hormonal component.
There will be a full assessment of you and baby including a 30-minute CTG to monitor baby’s heartbeat, and a discussion with the doctor. The Dilapan rods are then inserted into your cervix during a speculum examination, like a smear test, which is done by either your midwife or doctor. Up to 5 will be inserted and they slowly absorb the natural fluid in your cervix to expand over time. This opens your cervix and can encourage your body to release hormones in preparation for labour.
After 12-24 hours, the Dilapan rods will be removed, and your waters may be broken artificially. In approximately 2 in 10 pregnancies where Dilapan has been inserted, there may be no change in your cervix after the 12-24 hours. The doctor will discuss further options with you at that time which may include using Propess or Prostin, or the offer of a caesarean section, and they will recommend the most appropriate option based on your individual needs and safety.
What happens during an ‘Artificial Rupture of Membranes’ or A.R.M?
Artificial rupture of membranes (‘breaking your waters’) is when the midwife or doctor uses a narrow tool to break the bag of fluid around your baby. This can only be done if your cervix has already started to dilate (open) and requires the midwife to carry out a vaginal examination to check this. Sometimes we recommend breaking your waters after having Propess even if you are showing signs of labour.
You will be taken to a single labour room, your baby’s heartbeat will be monitored using a CTG for 30 minutes and then the midwife will examine you to break your waters. The baby will not be harmed by this. The procedure can be uncomfortable for you, speak to your midwife about pain relief options if you find examinations difficult.
We will check the colour of the waters and observe you for a short while afterwards. Ideally, regular contractions will start within 2-4 hours of your waters being broken. You will be offered a vaginal examination to see if your cervix has made any changes in that time frame, and if not, it is common for you to be offered the oxytocin hormone drip (called Syntocinon) for contractions to begin.
What is a Syntocinon drip?
Syntocinon is the synthetic (man-made) version of Oxytocin which is the hormone your body produces when it goes into labour. The Syntocinon is given through a drip (cannula) in your hand or arm and is used to start contractions.
Once the drip has started, we recommend monitoring your baby’s heartbeat continuously until the birth to make sure your baby is coping with the contractions. We will encourage you to be active during your labour, finding different positions that feel comfortable for you, and can help labour to continue.
You may wish to consider different pain relief options available to you when you are experiencing contractions with or without Syntocinon. Data shows there is an increase in the uptake of an epidural when having an induction of labour, but this is a personal decision. Please access some of the resources in the pain relief section below or discuss your options with a midwife or anaesthetic doctor during pregnancy or the induction process.
What are the risks of having an induction of labour?
Induction of labour is a safe procedure for you and your baby. However, there are a few associated risks.
- Hyperstimulation – With vaginal Prostaglandins or Syntocinon, the contractions may become too frequent (less than 60 seconds apart) or too long (over 90 seconds). This can cause your baby to show signs of distress. If this happens, the Propess can be removed, or your drip will be reduced/turned off to allow your baby to recover. If these steps are not effective, sometimes you will be advised to have an injection called Terbutaline to temporarily stop or slow the contractions. The IOL may be resumed after some time if considered safe for you and your baby, but in some cases, if your baby is unable to recover, a caesarean section may be advised.
- Symptoms – You may experience nausea, vomiting or diarrhoea after the Propess or Prostin is inserted. If this occurs, talk to your midwife who will discuss options with you as we may be able to provide medication to help with the symptoms experienced. It is also very common to experience heaviness in the vaginal area during the process, different positions can sometimes help with this.
For comparison of different types of birth e.g., assisted, or caesarean birth, please see the table near the beginning of this leaflet and ask any further questions to your midwife or doctor.
What are my pain relief options during an induction?
Like any labour, with an induction, you may experience significant pain during contractions. Everyone tolerates pain differently, but we have pain relief options available to you that you can request while you are having an induction. The different options are listed below, please discuss these options further with your midwife during pregnancy.
- Oral pain relief (tablets taken by mouth such as paracetamol, or liquid such as oral morphine)
- TENS machine
- Gas and Air (Entonox)
- Pethidine
- Epidural
Please use this link to access further pain relief in labour information on the LabourPains.org website (International translations available).
What is an ‘Outpatient Induction’?
You may be offered to have your induction started as an outpatient, which means having a Propess or Dilapan inserted in hospital, and then going home for up to 24 hours. There is quite a strict criterion for this, but please ask you midwife or doctor if this is something we can safely offer to you.
If you are suitable and are having Propess on the Day Assessment Unit, your midwife will book a date and time for you to attend (usually between 9 and 11am). If you are having Dilapan, or it is a weekend and you are having Propess, your midwife will book a date, and ask you to call the Maternity Helpline for a time to attend the Carmen Antenatal Ward.
The initial assessment, insertion and monitoring of baby will be the same as above. If everything is fine after the Propess or Dilapan has been inserted, you will be sent home, and advised to return the next day if there are no changes. If you experience any of the following, please call the Maternity Helpline (0208 725 2777) and come in to see us even if it is within the 24 hours:
- Fresh vaginal bleeding
- Reduced fetal movements
- Regular contractions
- Constant abdominal pain
- Waters breaking (clear/light pink waters)
- Waters breaking (brown/green if the baby has done a poo called ‘Meconium’ which is a concerning symptom)
- If the Propess or Dilapan rods fall out
- Or if you are worried about anything
Unfortunately, we cannot facilitate further parts of the induction process as an outpatient as it is not thought to be safe enough for you and baby, so you will be advised to have the rest of the process in the hospital where necessary.
What is an ‘Inpatient Induction’?
This is when the induction process is started in hospital, and you stay until the baby is born. If there are any concerns about baby, or your pregnancy has complex problems, this is what we will most likely recommend. If it is recommended, you will be booked in and given a date. Please call the Maternity Helpline at 9am on that day and our team will give you a time to come to hospital. Depending on your and your baby’s needs and risk factors, you will come to either Delivery Suite or Carmen Antenatal Ward.
In both locations, you will be given a bed in a shared room with up to 3 other people. There are privacy curtains, and we allow you to always have one person with you. Once labour is established, you are having your waters broken, or starting the Syntocinon drip, you will be moved to a single room.
On some occasions, your induction may need to be delayed due to the workload across the maternity unit. This is to ensure everyone is kept safe. Your midwife will discuss options with you and ensure you and your baby are well.
What should I bring?
Please bring your Antenatal Notes and your hospital bag with you, even if you are having an outpatient induction. From the start of the induction process, to going home with baby, sometimes parents can stay for up to 7 days. It is common to take 2-3 days for labour to start. There may be times where you feel frustrated that labour hasn’t started yet, please bring things that will help you feel busy. You can refer to page 14 in your Antenatal Notes for what to pack.
Do I have choices for my induction of labour and birth?
We want to support everyone to have a positive birth experience regardless of how their labour starts or where the baby is born. You may find this list helpful in thinking about choices for your birth. Your midwife and doctor will try their best to support your choices.
Gender: I already know my baby’s gender □
I would like to be shown my baby’s gender □
I would like my birth partner to tell me my baby’s gender □
I would like the midwife /doctor to tell me my baby’s gender □
Ambience: What music and lighting would you like?
___________________________________________________
Partner: My birth partner would like to cut the cord □
Extras: Vitamin K Oral □ Injection □
Delayed Cord Clamping □
Skin to skin: I would like immediate skin to skin with my baby □
I would like my baby to be checked first, then skin to skin □
I would like my birth partner to have skin to skin with my baby □
I don’t want skin to skin □
Who can I talk to about my options?
You can discuss the risks, benefits, and process of induction with any Midwife or Doctor during your antenatal appointments, or please call the Maternity Helpline (number below).
Open Monday – Sunday, 24 hours a day.
Maternity Helpline 0208 725 2777
If you have questions regarding place of birth or type of monitoring for baby, this may require a discussion with a Senior Midwife or Obstetric Consultant. Please ask for a referral to the Birth Options Clinic if you feel you would like to labour and birth outside of our routine guidelines.
If you would like to access the birth reflection service to discuss a previous birth experience during your current pregnancy or after your birth, please email the Professional Midwifery Advocates (PMA) pma@stgeorges.nhs.uk. You can also call them on 020 8725 2042 and leave a message with your name and telephone number for them to call you back.
Further information
National Institute of Health and Clinical Excellence (NICE) – NG207: Overview | Inducing labour | Guidance | NICE
Royal College of Midwives, Blue Top Guidance No.2 September 2019
NHS: Inducing labour
Tommy’s Charity: Inducing labour

