Is sugar driving the obesity epidemic?
The second-ever national Dietitians Week ran from June 8-12 this year with dietitians across the UK working hard to share their expertise and promote awareness for their role within healthcare.
As part of the week we joined forces with St George’s, University of London to organise a public debate about sugar. With numerous headlines stating that sugar is to blame for poor health, our dietitians wanted to set the record straight… or at least show that it isn’t quite as simple as some reports would have us believe.
Over 50 people attended the debate on June 11, but we know from twitter that there are many more of you out there who want to hear what was discussed. So with that in mind here is the summary of bariatric dietitian, Scott Lonnee’s presentation investigating whether sugar is to blame for the obesity epidemic:
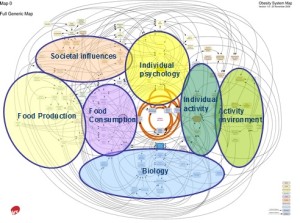
The cause of obesity is complex and multi-factorial. Sugar is associated with obesity however it is not an exclusive cause. As with incidence of overweight and obesity, sugar intakes vary across population demographics such as ethnicity, age group and socio economic status. For example, Germany, which ranks second globally in both sugar and fat consumption per capita, is among the skinniest nations in the developed world.
Proponents of reducing our ‘sugar intakes’ suggest that we should limit our consumption of ‘extrinsic’ sugars to no more than 10% of our total daily calorie intake. This is certainly good advice and in some population groups it may well stem the rate of weight gain, however in others it will have no impact at all.
It is recognised that the obesity epidemic is driven by simply eating too much of everything. That includes fats, sugars, carbohydrates, proteins and alcohol. Our modern food environment has changed to allow easy access to appealing energy dense foods at any given moment.
Modern life presents dietary options for rich foods, an increased frequency of eating and larger portions. Marketing of food appeals to our senses, such as value, opportunity, celebrations, condolences and avoidance of waste to name a few factors of influence. Food itself appeals to our psychology, to comfort us as medication. Foods also appeals to our knowledge of health and financial abilities to eat well.
No one single ‘advisory’ approach can hope to stem national weight progression. Obesity is classified as a disease and by observation; very few it seem can overcome and return to a healthy weight range. For those who do, durability of the weight loss becomes the main objective.
As varied as are the causes of obesity, so too are the solutions. Strategies need to be tailored to the individual. The first objective is to identify weight gain and halt progression. The next step is to consider barriers to weight loss and plan a strategy. The third stage is to monitor progress, compliance and to make changes and keep on track. If sugar reduction is identified as part of the plan then so be it.
In conclusion conventional wisdom prevails. Eat fewer calories (eat smart) and move more. The most important consideration is that the weight management plan is achievable and sustainable in the long term.