Normal Pressure Hydrocephalus
On this page:
St George’s Neurosciences Department provides a comprehensive regional and supra-regional service for managing Normal Pressure Hydrocephalus (NPH). We accept referrals from anywhere within England.
Dr Kuven Moodley and Dr Philip Fletcher run the neurology NPH clinic. Mr Timothy Jones, Ms Meriem Amarouche and Mr Erlick Pereira perform the ventriculo-peritoneal shunt insertion.
What is Normal Pressure Hydrocephalus?
Normal Pressure Hydrocephalus (NPH) is a brain disorder in which excess cerebrospinal fluid (CSF) accumulates in the ventricles (fluid-filled chambers inside the brain). Despite the excess fluid, the pressure measured during a spinal tap is often normal hence the condition being called Normal Pressure Hydrocephalus.
What causes Normal Pressure Hydrocephalus?
The majority of cases of NPH are of unknown cause. This is known as primary NPH. If NPH develops following a known cause such as head injury, subarachnoid haemorrhage, brain tumour, bleeding, infection or surgery on the brain it is then called secondary NPH.
What are the symptoms of Normal Pressure Hydrocephalus?
NPH is typically characterised by a triad of symptoms: difficulty walking, progressive metal impairment and dementia and impaired bladder control. These symptoms may not all be present to diagnose the condition. They can emerge at different stages of the disease with varying levels of severity.
Because these symptoms are like those seen in disorders such as Alzheimer’s or Parkinson’s disease, this can lead to a delay in recognising and treating NPH. Many cases go unrecognised and are never properly treated.
Why have I been referred to a neurosurgeon?
Once the diagnosis of NPH has been confirmed by your local neurologist or in the neurology NPH clinic at St George’s Hospital, you may be referred to a neurosurgeon to discuss surgical management.
The most common, and typically the only available treatment for NPH is the surgical implantation of a shunt. The most commonly used shunt for NPH is a ventriculo-peritoneal shunt (VPS). This diverts the flow of CSF into the abdominal cavity where it can be absorbed.
The VPS is made of three parts which are all implanted under the skin (Figure):
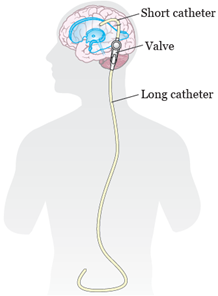
– A short or ventricular catheter: this is a flexible tube placed into the ventricular system of the brain;
– A valve: this is like a tap that helps regulate the amount of fluid that leaves the ventricles. We often use an adjustable valve which means that we can increase or decrease the flow of CSF through the shunt;
– A long or abdominal catheter: this is a flexible tube placed into the abdominal cavity.
The team at St George’s perform a significant number of these surgeries every year. When you are referred to Mr Timothy Jones or Ms Meriem Amarouche, they will see you in the outpatient clinic to discuss the diagnosis, the intended benefits as well as the possible risks of this procedure.
What is the prognosis after surgery?
The majority of those properly diagnosed with NPH and screened for shunt responsiveness will experience improvement in their symptoms. It may however take several weeks or months to see the full extent of improvement. Early diagnosis and treatment are often a better indicator of success but even patients who have had symptoms for many years may still improve with surgery.
There is however no known cure to NPH and the insertion of a shunt is performed to slow down the progression of the condition. Some patients may only notice a benefit for a few years.
When will I be admitted and discharged?
The surgery is performed at St George’s Hospital. You are likely to be admitted the day before your planned operation but we may ask you to come in on the day of the procedure. You will remain in hospital for at least one night after the operation. The next day, you will have a brain CT scan and Xrays of your chest and abdomen to confirm optimal placement of the shunt. You will be reviewed by a member of the neurosurgical team and most likely discharged home later that day. You may need to stay in hospital for a longer period of time if there are any surgical or medical issues that need to be addressed. This would be discussed with you/your family.
How will I be followed up after surgery?
You will have a clinic telephone follow-up four weeks after the surgery with a member of the neurosurgical team. The frequency of subsequent follow-ups will depend on whether your symptoms have improved or not. This shall be discussed in detail during your first appointment. Your follow-up will be predominantly with the neurosurgical team but you may be referred back to the neurology NPH clinic if further neurology input is required.
Referrals
What if I have any questions?
If your questions are not urgent please email hydrocephalus@stgeorges.nhs.uk. We will endeavour to get back to you within 3 to 5 working days.
If you think that you require urgent medical attention please do not use this email address and seek advice from your GP or nearest Accident and Emergency Department.


