Lymphoma
On this page:

Lymphoma is the 5th most common type of cancer in the UK. It is a cancer of the lymphocytes. Lymphocytes are a type of white blood cell that fights infection. Lymphoma develops when the lymphocytes become out of control. They divide abnormally or do not die when they should.
When you have lymphoma, abnormal lymphocytes can collect almost anywhere in your body. Lymphoma commonly develops in the lymph nodes in the neck, armpit or groin. It can also develop in the lymph nodes and tissues deeper inside your body; it can develop in the bone marrow.
In most cases, the cause of lymphoma is not known. Some people with conditions that affect their immune system have a higher risk of developing lymphoma—for example, people with HIV and those who have had organ transplants.
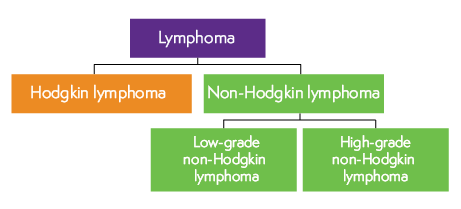
There are two main types of lymphoma: Hodgkin lymphoma and non-Hodgkin lymphoma (NHL). Within these types, there are many subtypes.
The Lymphoma Unit takes regional referrals and manages and treats complex and rare lymphomas, particularly T-cell lymphoma. St George’s provides a regional service for patients with HIV-related lymphoma and Kaposi’s Sarcoma. The lymphoma team and HIV specialist jointly review patients, and there are shared care arrangements for inpatients with the clinical infection unit.
What are the signs and symptoms?
The most common sign of lymphoma is a lump or lumps, usually in the neck, armpit or groin. These lumps are swollen lymph nodes, sometimes known as ‘glands’. Usually, they’re painless.
Other symptoms include fatigue; fatigue is different to normal tiredness. It means feeling exhausted for no apparent reason or feeling washed out after doing very little. They were losing a lot of weight quite quickly without trying to can be a symptom of lymphoma. Getting infections more rapidly and having difficulty getting rid of them can be a symptom of lymphoma. Sweats can happen at any time of the day with lymphoma, but they are most common at night. They are often described as ‘drenching’ and can make your nightclothes or bed sheets soaking wet. Itching, Itching (‘pruritus’) without a rash can be a symptom of lymphoma. It can be very uncomfortable, particularly when you get hot. Some people get fevers (temperatures above 38°C or 100.4°F). Fevers often come together with night sweats and weight loss, but they can happen separately. They can also be a sign of infection.
Do I need any tests to confirm the diagnosis?
Biopsy: This is a sample of tissue taken from your body and looked at under a microscope to check for abnormal cells. In most cases, a biopsy is the only way to confirm a lymphoma diagnosis.
Other tests help determine which part of your body the lymphoma affects. This is called ‘staging’. these include blood tests, scans such as a PET (Positron Emission Tomography) CT (Computerized Tomography) scan and sometimes times a bone marrow biopsy is needed.
A bone marrow biopsy is where a needle is used to take a sample of the bone marrow from the hip bone to look for any lymphoma cells.
Staging of lymphoma is the process of working out which parts of your body contain lymphoma. It is usually written as stage 1, 2, 3 or 4 or written in Roman numerals (I, II, III or IV). Most people with stage 1 or 2 lymphoma are said to have early-stage lymphoma. People with stage 3 or 4 lymphoma are said to have advanced-stage lymphoma. It is not uncommon for lymphoma to be advanced when it is diagnosed, as the lymphatic system is spread throughout the whole body.
Also, the letters A and B are often used to describe the stages of lymphoma. B means that you have unexplained weight loss, night sweats or fevers. A means that you do not have any of these symptoms.
What treatments are available?
Some people with lymphoma have regular check-ups after diagnosis but do not have treatment for lymphoma straightaway. This approach is called ‘active monitoring’, ‘active surveillance’ or ‘watch and wait’. Active monitoring might be suggestive if your lymphoma is slowly growing (low grade) and is not causing any troublesome problems. It does not mean that lymphoma cannot be treated, but there is no benefit to treating it until it causes problems that cannot be managed well.
Some lymphomas need treatment straight away. Treatment is usually with chemotherapy, antibody therapy (and other targeted therapy), radiotherapy or a combination of these. Lymphoma is sometimes treated using stem cell transplants.
There are many types of lymphoma treatment depending on the type of lymphoma that a patient has. More information can be found on the Macmillan and Lymphoma Action websites.
What is Personalised Cancer Care?
Personalised Cancer Care means your team will support you to take an active role in your cancer care by giving choices and control based on what matters most.
Together with your key workers’ team, like your Clinical Nurse Specialist and Macmillan Support worker, we will aim to help you access the care and support that meets your individual needs from the moment you receive your cancer diagnosis so that you can live as full, healthy and active a life as possible.
You will be invited to complete a Holistic Needs Assessment (HNA) to identify any concerns you may have when you have been diagnosed with cancer. These concerns may be physical, emotional, practical, financial and spiritual.
You will answer a simple set of questions or fill in a checklist about all areas of your life. It is to find out about the concerns you may have. You are often asked to rate how important these concerns are to you. It could help you decide what to discuss first during the assessment.
Once you have completed the assessment, your Clinical Nurse Specialist will discuss your needs, maybe face-to-face in a clinic or over the phone. During the discussion, you and your Clinical Nurse Specialist will agree on the best ways to manage your needs and concerns. They will write down what you have decided in a document called a care plan. They may write it during the discussion. Or they may make notes and send them to you afterwards. Your care plan will record the following:
- The main concerns you talked about
- Suggestions and actions to help you manage your concerns
- Services that may be able to support you, and any referrals that are made
- What is already being done to help – for example, the services you are already using
- Information about who to contact if you need more help
- The details of other health or social care professionals with whom you have agreed to share the information.
You may not wish to complete the holistic needs assessment at this time. The care you receive will not be affected in any way, and we will be happy to discuss this again in the future
Health and wellbeing information and support also include:
- Access to the Macmillan Information & Support Centre to find out what support is available in the community, e.g., practical, financial, and how to access it
- Help with understanding cancer and its treatment and how to manage its impact through videos and workshops run by healthcare professionals at St George’s and in the community.
- Attend wellbeing activities which are great opportunities for you and your carers to get together with others affected by cancer.